Introduction to Functional Endoscopic Sinus Surgery
Rhinology and sinus surgery have undergone a tremendous expansion since the discourses of Messerklinger and Wigand in the late 1970s.[1, 2, 3] Imaging advances, increased understanding of the anatomy and the pathophysiology of chronic sinusitis, and image-guided surgery have allowed surgeons to perform more complex procedures with increased safety.
Outstanding short- and long-term results have been reported in the literature. Senior et al reported that symptoms improved in 66 of 72 (91.6%) patients following endoscopic sinus surgery, with a mean follow-up time of 7.8 years.[4] In addition, endoscopic sinus surgery significantly influences quality of life; Damm et al reported an improvement in quality of life for 85% of their patient population, with a mean follow-up time of 31.7 months.[5] Although functional endoscopic sinus surgery is the primary approach used today for the surgical treatment of chronic sinusitis, the time-honored external approaches still play a role. Therefore, familiarity with endoscopic and external approaches, in conjunction with a precise understanding of the anatomy, ensures optimal patient care and outcome.
A recently developed alternative to functional endoscopic sinus surgery is balloon sinuplasty. This technique uses balloon catheters to dilate the maxillary, frontal, and sphenoid natural ostia without bone or soft-tissue removal. Reports show persistent patient symptom improvement and sinus ostia patency. Further study and long-term outcomes with this technology will determine its role in endoscopic sinus surgery.[6]
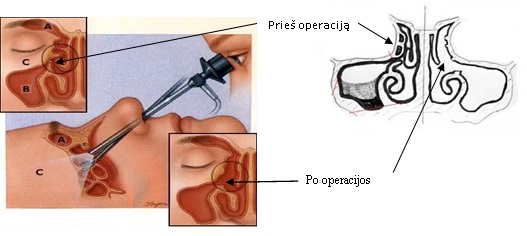
Endoscopic view of the paranasal sinuses before and after the FESS operation
- Endoskopinė sinusų operacija
- Endoskopinė sinusų operacija
- Kairio žandinio sinuso uždegimas
- Po operacijos. Bendras vaizdas
- Po operacijos. Iš arti
- Atvertas kaktinis sinusas
- Atvertas kaktinis sinusas
- Atvertas dešinys žandinis sinusas
Functional endoscopic sinus operation
Opening of frontal sinuses with sinus shaver Storz
Endoscopic treatment of chronic sphenoiditis on the left side
Removal of concha bullosa
FESS before and after the operation
Nasal endoscopy. Large nasal polyps
FESS. Widely opened frontal sinuses
Ethmoidectomy (polyps removal) using endoscope and shaver